Main Page
Welcome to the UCL High Energy Physics Group proton therapy Wiki.
This contains information on the various proton therapy-related experiments and software in use by the UCL High Energy Physics and Proton and Advanced RadioTherapy (PART) research groups.
This is subdivided into the following research areas:
- Proton Calorimetry: Development of a fast, accurate calorimeter module for high resolution proton energy measurements.
- Software: Instructions on installing and using the various pieces of software for simulation and analysis, including Geant4, FLUKA and ROOT.
Proton Beam Therapy

Modern cancer treatment is largely a combination of 3 techniques — chemotherapy, radiotherapy and surgery — each of which has associated advantages and drawbacks.
Conventional radiotherapy utilises X-rays with energies from 6 MeV to 18 MeV to irradiate cancerous regions of the body from multiple directions: the most modern variants of Intensity Modulated RadioTherapy (IMRT) provide a continuous intensity modulated X-ray beam through a full 360° arc, maximising the dose to the tumour whilst minimising the dose to the surrounding tissue.
The drawback of conventional radiotherapy is the amount of dose delivered outside the desired treatment region. At the energies used for radiotherapy, the peak energy loss for photons occurs within a couple of centimetres of the surface of the skin, with a slow reduction in energy loss as a function of depth. This unfavourable dose distribution is balanced somewhat by the multiple beam approach used in IMRT, but still leads to significant dose deposition in otherwise healthy tissue. This has particular significance in the treatment of deep-lying tumours in the head, neck and central nervous system, particularly for children whose bodies are still developing and are particularly susceptible to long-term radiation damage.
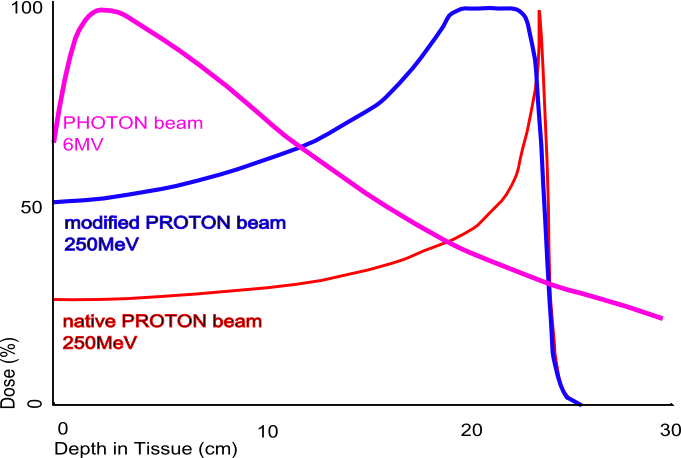
Proton Beam Therapy (PBT) is a more effective alternative to conventional radiotherapy, where high energy protons (60-250 MeV) are used in place of X-rays. The advantage of PBT is a consequence of the markedly different dose deposition profile of protons: as a result of the Bragg Peak most of the energy is deposited in the last few millimetres of the proton path. This allows a precise tuning of the delivered dose through appropriate selection of the proton beam energy and leads to much lower doses of radiation outside the target volume. Large-scale PBT facilities for cancer treatment are a new undertaking in the UK. The UK's only operational PBT centre is the Clatterbridge Centre for Oncology on the Wirral: with a 62 MeV cyclotron and a penetration depth less than 4 cm, treatment is limited to eye tumours.
Two new centres based at University College Hospital in London (UCLH) and the Christie Hospital in Manchester are currently under development. These will treat a total of 1,500 patients a year, primarily those with the most challenging tumours of the head and neck and the central nervous system.
To support these new treatment centres, UCL is engaged in a number of research programmes within both High Energy Physics and the UCL Dept. of Medical Physics to improve the quality of proton therapy treatment:
- Proton Radiography and Proton CT to provide better quality imaging.
- Proton and neutron dosimetry to maximise the clinical dose whilst minimising the damage to sensitive tissue.
- Throughput optimisation to enable a greater number of patients to be treated and greater flexibility of accelerator scheduling.
- Accelerator design and development for proton therapy.
For more information on Proton Beam Therapy research at UCL, please contact Dr. Simon Jolly.