Background/Cancer Therapy: Difference between revisions
SimonJolly (talk | contribs) No edit summary |
SimonJolly (talk | contribs) No edit summary |
||
| Line 47: | Line 47: | ||
=== Proton therapy === | === Proton therapy === | ||
[https://upload.wikimedia.org/wikipedia/commons/1/12/BraggPeak.png http://en.wikipedia.org/wiki/Bragg_peak] | |||
[[File:BraggPeakWikipedia.png|thumb|The dose produced by a native and by a modified proton beam in passing through tissue, compared to the absorption of a photon or x-ray beam|right|340px|link=http://en.wikipedia.org/wiki/Bragg_peak]] | [[File:BraggPeakWikipedia.png|thumb|The dose produced by a native and by a modified proton beam in passing through tissue, compared to the absorption of a photon or x-ray beam|right|340px|link=http://en.wikipedia.org/wiki/Bragg_peak]] | ||
Revision as of 15:36, 5 July 2017
The main aims of treatment are:
- Palliative — to relieve symptoms associated with cancer.
- Curative — to eliminate the cancer completely.
- Preventative — to reduce the risk of cancer recurrence.
There are a variety of different treatment options for cancer.
Surgery
Surgery is primarily reserved for solid tumours that are isolated to a particular location. Prior to surgery the tumour is often biopsied for laboratory analysis. This is done to allow the cancer to be staged (i.e: determine the severity of the cancer). If the cancer has not yet spread to other organs, the cancer can be completely excised (removed). Typically, an additional border is removed, around the tumour, to ensure no tumour is left behind. If the tumour has already metastasised, surgical excision of the tumour will not be curative and alternative approaches (perhaps in combination with excision of the primary tumour) will be considered.
Chemotherapy
Chemotherapy involves treating the cancer, typically over a number of separate sessions, using drugs (cytotoxic agents). Chemotherapeutic agents are fairly non-specific and target both healthy and cancerous cells, thereby causing a wide array of side-effects (including hair loss, nausea and fatigue).
The key to a successful chemotherapeutic agent is that it causes more damaged to cancer cells than it does to non-cancer cells. Most chemotherapeutic agents work by interfering with cell division (mitosis), because cancer cells have a high mitotic rate. Other cell classes such as hair follicle cells, or cells in the gut also have high mitotic rates and will inevitably be affected by the drugs.
Chemotherapy may be used to treat cancers that have already spread to other organs, unlike surgery, as the agents are distributed by the blood stream and can thus reach all tissues in the body. Chemotherapy is rarely used as the sole treatment for cancer and is often combined with radiotherapy or surgery.
There are several types of chemotherapy agents:
- Alkylating agents: these agents bind to DNA and will cause breakage of DNA strands during cell division. This can initiate apoptosis (programmed cell death).
- Anti-metabolites: these drugs may inhibit DNA synthesis, thereby preventing DNA replication during the synthesis (S) phase of the cell cycle.
- Anti-microtubule agents: microtubules are the major constituent of the spindle fibres involved in mitosis. Anti-microtubule agents interrupt the formation or disassembly of spindle fibres and thus interfere with the correct completion of mitosis. This causes cells to undergo apoptosis.
Targeted Therapy
The main problem with chemotherapy is the non-specific action of the drugs. Targeted therapy aims to minimise the damage to non-cancerous cells by targeting molecular processes/proteins specific to tumour growth and development. The side-effects associated with targeted therapies are fewer (and different) to those associated with traditional chemotherapy as healthy cells are damaged to a lesser extent. There are two main types of targeted therapy:
- Monoclonal antibodies: all cells express proteins (receptors) on their surface. Cancer cells may express abnormal or different/upregulate the expression of specific receptors. These receptors can be targeted specifically by a ligand. If this ligand is bound to a toxin, the target cell can be killed.
- Small molecule inhibitors: these targeted therapies use small molecules that can gain entry into cancer cells, disrupt the internal metabolic pathways and cause cell death.
Radiation
Radiation therapy works by inducing damage to the DNA of cancerous cells, with the aim of causing cell death. It is important to limit the radiation dose to healthy cells to prevent un-necessary damage to such cells. The radiation source is typically high-energy X-rays (especially for external beam radiotherapy) but can also be gamma radiation.
Brachytherapy
Brachytherapy involves the placement of a sealed radiation source, inside, or extremely close to the tumour, under image guidance. Through careful planning of the placement of the sealed sources, the radiation dose to the tumour can be kept high whilst maintain the radiation dose to healthy organs and tissues within certain tolerance limits.
External beam radiotherapy
External beam radiotherapy involves using a high-energy radiation beam generator (a linac – linear accelerator). The linac rotates around the patient and a number of different radiation beams (from a range of different angles) are applied. All the beams centralise on the tumour (the isocentre). Thus, the radiation dose to the tumour is higher than the radiation dose to any other organ or tissue. The shape of each individual beam can be carefully controlled to minimise the radiation exposure to healthy tissues, or highly radiation-sensitive organs such as the spinal cord.
In radiotherapy, the energy of the radiation is deposited within tissues slowly. As the radiation passes through the tissue, the radiation energy is transferred to cells and is lost from the primary beam. As such, at a certain depth there will no longer be any energy in the radiation beam. However, almost all the cells along the radiation beam will experience a certain radiation dose (surface skin cells may be spared a radiation dose — the effect is termed the skin-sparing effect).
Proton therapy
http://en.wikipedia.org/wiki/Bragg_peak
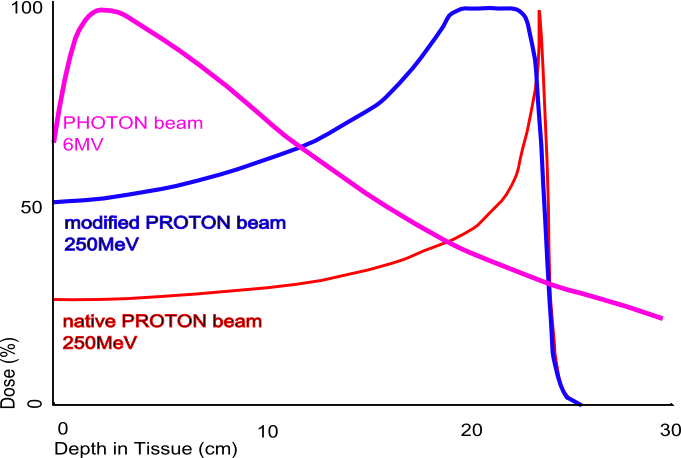
This is a type of radiation treatment that utilises protons rather than x-rays or gamma rays to treat cancer cells. Protons are positively charged particles. They can be accelerated to very high energies in a cyclotron. After gaining a sufficient amount of energy, the protons will be capable of destroying cancer cells. Unlike radiotherapy, protons will not deposit there energy slowly, and continuously as they traverse the patient. Instead, they deposit the vast majority of their energy in one go, at a particular depth. The depth at which most of the proton energy is deposited can be determined from the Bragg curve of the proton (by the presence of a Bragg peak), which depends on the initial proton energy. Although the quantity of radiation delivered to cells after the Bragg peak is almost 0, the quantity of radiation prior to the Bragg peak is not. Thus, there will still be some radiation dose, albeit fairly low, to some non-target cells.
Proton therapy allows much greater control over the location of the delivery of the radiation and therefore permits the delivery of a much lower radiation dose to healthy tissues and cells than conventional external beam radiation therapy. Typically a number of different protons of different energies will be used to treat a tumour.